Cost and environmental impact are key concerns
Some endoscopes—the long, thin tubes with a camera at one end used for many diagnostic procedures—are used and then thoroughly cleaned and disinfected for reuse. Others are designed to be used once and discarded. As the camera quality improves, deciding which tool to use is a matter of weighing cost, time, infection rates and environmental impact.
FDA’s recommendation to make the switch
Single-use or disposable endoscopes hit the market more than 20 years ago. Their popularity has exploded over the last five years as costs have come down and image quality has improved.
In April 2022, the U.S. Food and Drug Administration (FDA) issued guidance that healthcare facilities should work to transition from using duodenoscopes with fixed endcaps to ones that are either fully disposable or made with disposable components. This is due to sanitation concerns and contamination rates with fixed endcap duodenoscopes. The FDA’s rationale is that disposable duodenoscopes eliminate the need for reprocessing and bring the contamination rate from as high as 6% down to just 0.5%.

Some duodenoscopes with fixed caps were pulled off the market due to problems with cleaning. “Because of the way it is designed, an endoscope is a complex piece of equipment. There are a lot of areas where bacteria and other contaminants can get trapped,” says Karen Bush, MSN, FNP, BC, NCRP, former Director of Clinical Research & Education at HealthTrust. “An endoscope’s design is so complex that proper handling and care are very difficult, with a massive number of steps to reprocess them.”
Each model has different cleaning procedures, and staff must receive training and stay up to date with continuously changing processes. The FDA recommends single-use endoscopes because the process to clean endoscopes can be quite cumbersome and difficult to follow.
Weighing infection risk

Single-use endoscopes are appealing for several reasons. For infection prevention, single-use scopes’ most attractive quality is that there is no risk of transmissible disease. “The infection risk of getting a communicable disease from a reusable endoscope is statistically low, but what if you can make the risk zero?” says William Cloud, M.D., MACM, CBBC, Chief Medical Officer at Baptist Memorial Health Care and a general surgeon with 35 years of experience.
The issue is more prevalent in endoscopes used for digestive procedures because there is a transmission risk from patient to patient and from patient to staff. “Common things that get transmitted with a gastrointestinal scope that we worry about are hepatitis A and E. coli,” says Dr. Cloud. “With bronchoscopes, we worry about tuberculosis and bacterial infections.”

Gregory Neal, M.D., is a general surgeon at The Surgical Clinic, a network of private practice surgeons in Middle Tennessee. In his 25 years in practice, he’s done upper and lower endoscopies looking for gastric cancers, reflux issues and ulcers, as well as surveillance and diagnostic colonoscopies.
About 15 years ago, a community hospital where he was working had a problem with their bronchoscopes. The infectious disease team found contamination putting patients at risk. Related to a design change in the bronchoscopes a few years prior, one of the parts wasn’t getting disinfected properly due to a manufacturing defect. “We had to go back to the manufacturer, and it revised the cleaning process,” says Dr. Neal. The New England Journal of Medicine published the study.
Evaluating cost
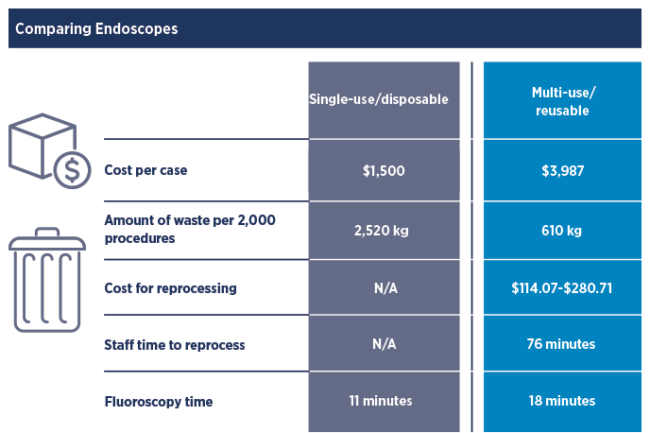
Hospitals should consider the long-term costs associated with reusable scopes when weighing the decision to move to disposable endoscopes. Staff time associated with disinfecting, the risk of disease transmission and the costs to repair must all be examined closely and compared with the costs of single-use scopes.
Reprocessing scopes can cause delays. “We started using single-use scopes because processing inefficiencies were causing delays in care,” says Dr. Cloud. “Urologists would need to scope a patient at the bedside or in the ED, and there wasn’t a cystoscope available because it was being processed, or there wouldn’t be staff available to process the scope in time for the next patient.”
In 2017, the International Association of Healthcare Central Service Materiel Management (now the Healthcare Sterile Processing Association) published the results of a pilot project that looked at the true cost of reprocessing endoscopes. In a detailed analysis that is publicly available online, the study’s authors found that the time it takes to reprocess one flexible endoscope is approximately 76 minutes of hands-on staff time, and the cost to do this work ranges from $114 to $280 per scope. These findings demonstrate the significant amount of time and effort associated with endoscope reprocessing. “It shows that single-use scopes may be either equivalent or even slightly cheaper than reusable scopes,” adds Dr. Cloud.
Regulatory agencies like The Joint Commission hold hospitals and surgery centers accountable for meeting quality standards. “They want to look at your scope cleaning and reprocessing [during visits] and make sure you’re using the manufacturer’s recommended process,” says Dr. Cloud. The manuals are 50 pages long, and it becomes a difficult compliance challenge to train staff and keep them up to date on the appropriate processing for all scopes. “These agencies want to ensure you’re doing it correctly, but the amount of education and experience required to maintain competency is considerable.”
Because reusable endoscopes require stringent cleaning and reprocessing that can involve pages of instructions, there are associated labor, repair, training and education costs that don’t exist for single-use endoscopes. Reusable endoscopes may seem less costly than single-use, but once a hospital or surgery center considers all factors,
the cost per case may be lower for single-use, depending on patient volume. A reusable scope might have an average lifespan of six years, after which users start to see a reduction in image quality and a decline in maneuverability.
At Baptist Memorial, staff are currently using single-use cystoscopes and bronchoscopes. The leadership team there acknowledges that this is the direction the industry is headed. “We are costing it out and seeing that the image quality is now there, the upfront costs are lower, there is zero risk of communicable disease transmission, and you don’t have to pay for cleaning and reprocessing,” explains Dr. Cloud. These factors mean looking at the problem with a fresh perspective.
Hospital setting vs. ambulatory surgery center
“Single-use endoscopes are an emerging technology. When we start to compare cost, reimbursement and location, it may be a less costly system,” says Dr. Neal. Using a disposable system gives a surgical team different options for where an endoscopy is performed. “It comes down to cost and patient affordability. An ambulatory surgery center (ASC) is cheaper than going to a hospital and a clinic would be even more economical.”
Determining the best path for your organization depends on a lot of variables. If you’re running a hospital versus an ASC, the utilization rate for patients will be different. “ASCs are mainly doing elective procedures, so a lot of the efficiency factors that have to do with bedside scopes aren’t an issue there. And, an ASC may not have the purchasing power to afford the upfront costs of single-use endoscopes, so it’s important to run the numbers. An ASC with a national footprint may be able to get good prices and make a difference,” Dr. Cloud explains.
 “If you’re a larger health system, you can buy a larger quantity and get products at a lower cost, whereas some ASCs that are on their own aren’t going to see enough volume to justify the cost,” says Bush. An ASC usually has dedicated staff to do these procedures regularly, but they may not have the physical space to store single-use endoscopes. AdvantageTrust members could benefit by optimizing use of contracted items through HealthTrust.
“If you’re a larger health system, you can buy a larger quantity and get products at a lower cost, whereas some ASCs that are on their own aren’t going to see enough volume to justify the cost,” says Bush. An ASC usually has dedicated staff to do these procedures regularly, but they may not have the physical space to store single-use endoscopes. AdvantageTrust members could benefit by optimizing use of contracted items through HealthTrust.
Environmental concerns
There is one significant concern with single-use endoscopes: negative environmental impact. “I worry about the waste of the equipment,” says Dr. Neal. Single-use endoscopes increase the volume of medical waste that a hospital must manage. Even though some components can be recycled, the cost of running recycling programs can be substantial.
Endoscopy is a substantial contributor to medical waste in the environment. In a 2022 study published in the leading international BMJ journal Gut, scientists looked at the environmental impact of the U.S. healthcare industry switching from reusable endoscopes to their disposable counterparts.
The study authors found that each endoscopy generates roughly 4.6 pounds of disposable waste, which adds up to about 38,000 tons of estimated total waste generated from all endoscopic procedures performed in the U.S. annually. That’s the equivalent of 25,000 cars.
The study showed that the environmental impact of endoscopes is significant, and transitioning to single-use endoscopes may reduce reprocessing waste but would increase net waste by 40%—and increase the cost of waste management.
To learn more about moving to single-use endoscopes, email clinical.services@healthtrustpg.com
The disposable endoscopes category contains ear, nose and throat scopes; duodenoscopes; bronchoscopes; rhinolaryngoscopes; ureteroscopes and intubation scopes. Vendors currently on contract with HealthTrust include:
- Ambu #64973
- Bard Medical #65488
- Boston Scientific #65423
- InterMed Resources #72464
- Karl Storz Endoscopy-America #65426
- Verathon #65429





